If you’re a prostate cancer survivor who has had his prostate gland and surrounding tissue removed in a radical prostatectomy, you know this condition can profoundly affect your quality of life.
Urinary incontinence is a potential byproduct of this procedure, combination therapy (chemotherapy and hormone therapy) and radiotherapy. You might find yourself avoiding sexual intimacy, general exercise and favorite physical activities such as golf or tennis. You might even sacrifice your social life because you’re hesitant about being out in public.
Wearing uncomfortable pads or diapers can make you self-conscious, too. No one wants to experience the embarrassment of smelling of urine or having a leakage accident in public.
“Don’t let this condition make you become homebound, isolated and depressed,” says Dr. Richard Kershen, a board-certified urologist at Hartford HealthCare’s Tallwood Urology & Kidney Institute. “Urinary incontinence is curable.”
Prostate cancer is the second-most common cancer among American men, after non-melanoma skin cancer. More than 172,000 men were diagnosed with prostate cancer in the United States in 2014, the latest figures available from the Centers for Disease Control and Prevention. Of those, an estimated 138,000 have their prostate gland removed in a prostatectomy. Many experience urinary incontinence, usually short term. For others, however, lasting incontinence can disrupt their daily lives.
The Post-Prostatectomy Rehabilitation program at Hartford HealthCare’s Tallwood Urology & Kidney Institute has the latest diagnostic tools and therapeutic technologies for quick and precise diagnosis, followed by a detailed treatment plan.
“Our mission,” says Dr. Kershen, “is to restore urinary control and sexual function after a radical prostatectomy and meaningfully improve your quality of life.”
Why Do Patients Suffer Urinary Incontinence After Prostate Removal?
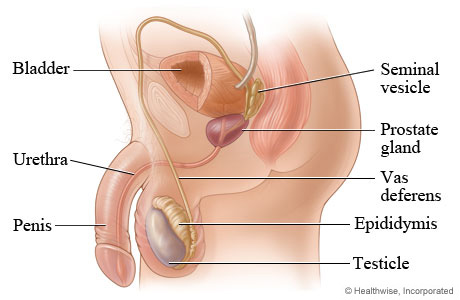
Even with the best medical care, up to 40 percent of radical prostatectomy patients might experience some degree of urinary incontinence. Why? The prostate gland is an integral part of the internal urinary sphincter mechanism that controls the flow of urine from the bladder into the urethra.
With the prostate removed, urinary control becomes largely dependent on the lower external urinary sphincter that has been left behind. In some patients, this external sphincter cannot fully compensate for the loss of the internal sphincter (prostate), causing incontinence.
Types of Urinary Incontinence
Male Stress Urinary Incontinence (SUI): Involuntary urine leakage that usually occurs with activity or physical exertion. It’s caused by external forces or pressure applied to the bladder that overcomes a weakened urethral sphincter, allowing urine to be expelled involuntarily.
It’s the most common type of urinary incontinence men experience after radical prostatectomy.
This type of leakage also develops sometimes after a transurethral prostatectomy (removal of a portion of the prostate gland through the urethra), “simple” prostatectomy (removal of only the part of the prostate blocking urine flow) or benign prostatic hyperplasia, also known as benign prostatic hypertrophy (a noncancerous enlargement of the gland).
The degree of SUI after prostate removal can vary widely.
Some men may leak only a few drops with heavy physical exertion. Others may be completely incontinent, with continuous urine leakage resulting from even a simple act like standing up. Most men with SUI after prostate removal have mild to moderate leakage, usually occurring with coughing, sneezing, bending, lifting or exercise.
Rarely, men have more severe incontinence with little or no urinary control. They leak continuously while standing, with little to no sensation. Whether you leak just enough to need one pad per day or experience severe leakage requiring diapers, effective treatments are available.
Urgency Urinary Incontinence (UUI): Urgency Incontinence is the involuntary loss of urine, usually after a strong, sudden need to urinate. This type of incontinence is often associated with other symptoms of overactive bladder, such as urinary frequency (voiding more than eight times per day), urgency (the feeling that you may leak if you don’t void immediately) and nocturia (awakening more than once per night to void).
It is most commonly caused by involuntary contractions or “spasms” of the bladder and may be associated with severe sudden episodes of incontinence with little to no warning or activity. If your prostate cancer was treated with radiation therapy, either alone or in combination with surgery, you are more likely to suffer from urgency incontinence than men who have had only surgery.
Mixed Urinary Incontinence: Unfortunately, some men suffer both stress and urgency urinary incontinence. Leaking can be caused by a cough, sneeze or physical exertion. They’ll also experience strong, sudden urges to void and often not make it to the restroom in time.
Climacturia or “Orgasmic” Incontinence: After a radical prostatectomy, you might leak urine when sexually excited and also eject urine from the urethra during orgasm. This commonly occurs along with stress urinary incontinence, frustrating both you and your partner.
Personalized Evaluation
We know it takes a lot of courage to seek treatment for incontinence. You may be suffering from more than one urinary symptom or condition. Every patient is different.
We’ll review your medical records and operative reports prior to your visit with us. At your initial visit, we will discuss your history with you and perform a detailed physical examination.
We generally recommend four tests to determine the nature and severity of your incontinence:
Three-Day Intake and Output Voiding Log: This is a log maintained at home on three separate days, consecutive or nonconsecutive. You’ll record all fluid intake as well as keep track of the time of day and volume of your individual urine voids. You’ll also keep track of any leakage episodes and what you were doing when they occurred.
Three-Day Pad Weight Test: Collect your wet pads for three days and seal them in storage bags, then bring them to your next appointment along with an identical dry pad. We will weigh them to obtain an estimate of your average volume of urine loss per day. Alternatively, you may obtain a kitchen scale (grams) and weigh your pads at home. Don’t forget to subtract the dry weight of the pad.
Urodynamic Testing: This test, performed in our office, provides a physiologic recording of your bladder and urinary sphincter function. This gives us a precise determination of the nature and cause of your urinary incontinence and any other bladder symptoms which you may have.
Flexible Cystoscopy: This is a three-minute, visual inspection of your bladder, urethral sphincter and urethra using a high-definition, fiber-optic camera. We can observe directly any anatomic abnormalities that may be affecting your urinary function.
Individually Tailored Care and Treatment Plan
Once we have all of your information -- including your history (both medical and surgical), your voiding log, pad test, urodynamic evaluation and cystoscopy -- we develop individualized treatment recommendations to maximize your dryness and minimize any potential side effects that may result from treatment. We always strive to come up with a plan that will alleviate your most bothersome complaint in the most expeditious way possible.
Effective Treatments for Male Stress Urinary Incontinence
AMS AdVance Male Sling System
The AdVance Male Sling, a strip of soft mesh placed inside the body, is designed to stop leakage by supporting the sphincter muscle. The AdVance Male Sling, available since 2003, moves the sphincter back to its natural position to help restore bladder control. It requires no action by the patient to function.

AdVance Male Sling Facts:
- Placed entirely inside the body, undetectable.
- High success achieved in most patients with mild to moderate incontinence and in selected patients with severe incontinence.
- Most patients greatly improved or totally continent immediately following the procedure.
- Operates on its own to restore continence.
- 92 percent of patients say they would undergo the procedure again.
The Procedure: The sling procedure, performed under anesthesia, is usually done on an outpatient basis. Your doctor accesses the urethra and the urinary sphincter through small openings.
Then the sling is placed under the urethra and tensioned to reposition the urethra, optimizing the sphincter’s function. Most patients are continent immediately following the procedure and can resume normal, non-strenuous activities within a few days.
The AMS 800 Artificial Urinary Sphincter Urinary Control System
The AMS 800 Urinary Control System -- also called the Artificial Urinary Sphincter (AUS) -- provides proven, discreet bladder control. This system, available for more than 40 years, is widely considered the best treatment for male stress urinary incontinence.
 The AMS 800 offers men with the most severe incontinence an effective and durable cure, dramatically improving their quality of life. The device, implanted surgically using small incisions, includes a pump (implanted in the scrotum), an inflatable cuff (placed around urethra) and a balloon reservoir (implanted in the abdomen).
The AMS 800 offers men with the most severe incontinence an effective and durable cure, dramatically improving their quality of life. The device, implanted surgically using small incisions, includes a pump (implanted in the scrotum), an inflatable cuff (placed around urethra) and a balloon reservoir (implanted in the abdomen).
The AMS 800 System, filled with saline, uses fluid hydraulics to open and close the cuff surrounding the urethra. When you need to urinate, squeeze and release the pump in the scrotum several times to remove fluid from the cuff. When the cuff is empty, urine can flow out of the bladder. The cuff automatically refills in a few minutes, squeezing the urethra closed to restore bladder control.
AMS 800 AUS Facts:
- Mimics a healthy sphincter, allowing you to urinate when desired.
- Works in the most severely incontinent patients.
- 90 percent of patients satisfied.
- 92 percent or more would have the device placed again.
- 96 percent or more would recommend the device to a friend.
The Procedure: The AUS procedure can be performed on an outpatient basis or may require a short hospital stay. Small openings are made near the scrotum and below the abdomen to insert an inflatable cuff, a pump and a small, pressure-regulating balloon. The surgery is performed under anesthesia.
Four to six weeks after surgery, you’ll return to our office to have the AUS activated and learn how to use the device.